This blog is created to share the experience of ENT Surgeon and to discuss things commonly discussed in clinic and is not available on professional websites
Sunday, November 16, 2014
Friday, October 10, 2014
Tuesday, October 7, 2014
Saturday, September 27, 2014
Red flags in oral submucous fibrosis
Pain
Bleeding
Halitosis
Loose teeth
Recent onset trismus
These are red flags to suspect malignancy in Oral sub mucous fibrosis.
Tuesday, September 23, 2014
Leukoplakia of tongue
I
Monday, September 22, 2014
Sunday, September 21, 2014
Friday, September 12, 2014
Bilateral thick tympanic membranes with normal middle ear
 |
| Note thickened ear drum on both sides with normal middle ear and mastoid air cells. |
 |
| HRCT Temporal bone-Axial cut. Double click to see whole CT. |
The author describes a unique case of bilateral thick tympanic membrane (ear drum) with normal middle ear and air cells.
The patient (50 years male) presented with decreased hearing both sides for last few years. He was treated for otitis media with effusion or white debris in his ear canal with good result. During his last visit, the author noticed that his normal ear drums don't have any landmark and has pink red mucosal color. A high resolution temporal bone CT was down.
Thursday, September 11, 2014
Sunday, September 7, 2014
Post traumatic hematoma with perichondritis with resultant cauliflowerdeformity
 |
| Post traumatic hematoma and then perichondritis of pinna which was solely treated by oral antibiotics by general surgeon. |
 |
| Thickened pinna as seen from behind in a case of post traumatic perichondritis. |
 |
| Three incisions were given to drain the hematoma and infected material. two quilting sutures were given to keep the dead space minimum inside. |
 |
| Same patient with non tender pinna after 2 weeks of surgical treatment coupled with antibiotics. |
 |
| Same patient as above after surgical treatment. See the irregular surface persisting resulting in cauliflower deformity. Patient in pain free now. |
Tuesday, September 2, 2014
Wednesday, August 27, 2014
Expert comments about loss of cervical lordosis on x-Ray
36 yr male with feature suggestive of imbalance while walking.
Daily drives 3 hrs
Comments:-
Radiologist
People get x ray cspine done for vertigo... But it's useless
Spondylosis is the rarest of rare causes of vertebrobasilar insufficiency
I guess that guy might be having labyrinthitis... Give him vertin and send him home 😐
ENT
It's clear cut case of loss of cervical lordosis. Radiologist have reported it as normal. This suggests early cervical spondylosis. I have an argument with him. That's why I wish to have your view on this. But you don't digest anything below MRI. 😄
Radiologist
Lol.. Loss of cervical lordosis is physiological mostly... What we tout as clinically relevant finding is mostly bullshit... Telling u by experience. The rad is right... Don't argue...
And spondylosis WONT cause imbalance
ENT
😐
Radiologist
The patient is only 36 and if the disc spaces are not reduced... Then don't call spondylosis just bec of the straightening...
In the US we call it musculoligamentous sprain/ spasm.. It's also a rare entity but we have to use it all the time in all patients mostly... It sucks big time!
Neurosurgeon
In case of muscle spasm
... u get this pic.its only suggestive of music spasm.....a natural protective phenomenon.
Muscle
Apply collar.
Symptatic tt.
if no relief....mri
Radiologist
Yes.. But in MANY MANY normal patients too you get this finding .. It's hugely non specific
Neurosurgeon
Yes
Radiologist
Pt presented with vertigo/ imbalance. Only in appropriate clinical setting it shud be called spasm... It's not a feature of spondylosis
ENT
Ok. That was one issue about finding of loss of cervical curvature which you say is not a feature of spondylosis.
Second association of spondylosis with imbalance.
Or spasm with imbalance
Pediatrician
In cervical spondylosis also some pt complains of giddiness.... Subjective....xray protective muscle spasm...relieve with muscle relaxant. No role of cervical collar I think..needs. Neurologist's expert view.
Neurologist
Hi. Xray definitely cervical spasm. Diagnosis- IT Professional😂
Collars are contraindicated
Rx. Symptomatic only
Radiologist
And FYI... If u see any child's x ray/ MRI.. The curvature will be straightened or reversed. Just letting u know....
I wish to thank Dr. Shivram Gopal Iyer, Dr. Amit Gupta, Dr. Gautam Tripathi, Dr. Rupesh Jain for participating in discussion.
Please leave your comments or questions for panel to answer.
Tuesday, August 26, 2014
Informed consent for endoscopic sinus surgery
Informed Consent for
ENDOSCOPIC SINUS/NASAL SURGERY
(Approved by All India Rhinology Society)
son/daughter/wife of:
Age &sex:
Reg.No.:
Address
PLEASE READ THIS DOCUMENT CAREFULLY AND ASK ABOUT ANYTHING YOU DO NOT FULLY UNDERSTAND. AFTER YOU HAVE READ IT, PLEASE SIGN FOR THE SURGERY OR PROCEDURE.
1. I have spoken to the doctor (s) who has/ have explained that I/my have/ has (condition/symptoms/provisional diagnosis)
2. What might happen to me/my if we do not treat this condition has been explained to me. The different ways to treat the conditions and the advantages and disadvantages of each of these was discussed with me. The Doctor has informed me that my problem may have arisen as a consequence of an allergy and has accordingly asked me to be treated for it as the surgery itself is only a part of the treatment.
3. The doctor wants (suggested) me/ my to have the following operation (s) or procedure (s): ESS/Septal Surgery/Turbinate Surgery
4. The doctor talked to me about how this surgery or treatment might help me. The doctor explained that the treatment might change if there was a change in my condition or if they find something different during treatment. The doctor also told me about how long it would take me to recover.
5. I am fully aware that the treatment/ surgery/ procedure is being performed in good faith and no guarantee/ assurance has been given as to the result that may be obtained. The doctor gave me an opportunity to ask questions about my condition and different ways to treat it.The doctor answered my questions. I am satisfied with the answers about my treatment.
6. I have been fully explained that there can be risks, complications or side-effects about any operation or medical procedure or anaesthesia. I know the doctor cannot tell me about every possible risk, complication or side-effect. We did talk about the major ones (for example : bleeding, infection, pneumonia, heart complications, blood clots, risk to life) that could happen if I have the operation or procedure. However the chances of these major complications are very rare. One to two percent of the patients can have bleeding which may require controlling it under anesthesia.
7. The doctor also explained me about these other risks :severe bleeding possibly requiring transfusions and possibly leading to stroke and/or death, bleeding into the eye and/or brain requiring external incisions for drainage, persistent nasal crusting, persistent tearing and/or damage to the tear ducts, damage to the nasal septum including hole formation in the septum, numbness and/or chronic pain to the forehead, face, and/or teeth, new or persistent infection with possible spread or infection to form brain infection or abscess, loss of or damage to sense of smell and/or taste, eye infection or abscess, and infection in distant spots of the body, damage to the eyes including permanent blurred vision and/or blindness, brain damage including damage to the lining of the brain, temporary or permanent scarring of the sinuses, with brain fluid leak, the need for further sinus, eye, or brain operations including operations that lead to external scarring, heart attack, stroke and/or death, and other unanticipated risks. Again these complications are extremely rare.
8. The doctor gave me a chance to ask questions about these risks and any other risks I wanted to know about. The doctor answered my questions. lam satisfied with the answers about the risks.
9. The doctor has explained to me that the doctor or whosoever may be designated as assistant may be doing important tasks related to surgery or procedure under the direction of the doctor.
l0 This surgery will be performed under local/ general anaesthesia.The doctor has explained to me about the general/complications of drug interactions, blood transfusion and risk to life.
11. If something unexpected happens or is found during the procedure or operation, that in the doctors opinion. Pose an immediate and substantial risk to my health and needs treatment in addition to or different from what is described above, also agree that the doctor (s) may at that time provide the treatment that is immediately necessary.
12. In the event of any systemic complications, I authorize the doctor (s) to transfer the case to an appropriate medical centre for necessary treatment.
13. Any tissues or parts surgically removed may be sent for examination/disposed off in accordance with accustomed practice.
14. I consent to pictures or videos being recorded or televised during my treatment for medical, research or educational purposes, as long as my identity is not shared.
l0 This surgery will be performed under local/ general anaesthesia.The doctor has explained to me about the general/complications of drug interactions, blood transfusion and risk to life.
11. If something unexpected happens or is found during the procedure or operation, that in the doctors opinion. Pose an immediate and substantial risk to my health and needs treatment in addition to or different from what is described above, also agree that the doctor (s) may at that time provide the treatment that is immediately necessary.
12. In the event of any systemic complications, I authorize the doctor (s) to transfer the case to an appropriate medical centre for necessary treatment.
13. Any tissues or parts surgically removed may be sent for examination/disposed off in accordance with accustomed practice.
14. I consent to pictures or videos being recorded or televised during my treatment for medical, research or educational purposes, as long as my identity is not shared.
Monday, August 25, 2014
NASAL POLYPS WITH ORBITAL INVOLVEMENT
NASAL POLYPS WITH ORBITAL INVOLVEMENT
Dr. V. P. Sood New Delhi.
Past President : Association of Otolaryngologists of India.
Past President : All India Rhinology Society.
Although patients with nasal polyps are common in E.N.T. practice but the aetiology of this condition still remains a mystery. The etiopathogenesis of nasal polyps has long been a subject of study, yet there is little agreement as to the mechanism of polyp formation. So far two main theories have emerged, allergic & infectious. Recently, sensitivity to aspirin and fungal infections have also been implicated as etiologic factors. Nasal polyps has been referred to as "benign allergic polyps" but research suggests that they are not more common in allergic patients. But now allergy has again been considered and there is a possibility that localized nasal allergy may have a role in the aetiology of polyps. The role of fungal infection in the aetiology of nasal polyps has been the source of great debate amongst rhinologists, since allergic fungal sinusitis has recently come to limelight.
In long standing infective polyposis most of the time there is bony necrosis of medial wall of maxillary sinus, lamina papyracia, ethmoid cells and anterior wall of the sphenoid sinuses. Chronic infective polyps degenerate to form into cheesy and muddy material, a condition referred to as necrotising ethmoiditis which should rather be called necrotising sinusitis since disease process is not only localized to ethmoid sinuses but can involve all the sinuses. The extent of endoscopic surgery should be planned and adapted to the requirement of individual cases. For circumscribed pathology minimum invasive endoscopic interventions are indicated. For diffuse polyposis of all sinuses a complete endoscopic ethmoidectomy together with the fenestration of the frontal, sphenoidal and maxillary sinuses is done. The disease is cleared from within the sinus cavities through the enlarged opening of the respective sinus. The end result should be as open ethmoidal cavity lined by moist mucosa and having free communication with the frontal, sphenoidal and maxillary sinuses. In multiple nasal polyps initial clearing is generally done with the help of microdebrider. Surgical results improve by carefull pre-operative planing, use of systemic antibiotics and steroids pre and post operatively. Use of thru-cut forceps and microdebrider also helps to preserve mucosa to achieve better results. Reconstructing adequate antrostomy is also conductive for better results. In diffuse polyposis a short course of systemic steroids pre operatively and post operatively is mandatory followed by topical steroid sprays.
Local application of amphotercin-B is now used especially when polyps are associated with fungal infections. Even in extensive polyposis, I prefer to do endoscopic sinus surgery under L.A. because the pupillary reflexes can be monitored and patient's subjective feedback of excessive pain sensation when the instruments are touching the orbital plate, cribriform plate or fovea ethmoidalis can be warning signals to the surgeon, which increase the safety index in endoscopic sinus surgery. I follow up my patients endoscopically for suction clearance of crusts and discharge. If I find any adhesion in middle meatus that is incised. If any small polyp is visible that is also removed without any pain or discomfort to the patient.
The follow up of patients in our country is poor. Patient must be told about importance of follow up. Modem technology, CT scanning and endoscopy enables us to make an early and appropriate diagnosis of nasal polyposis and Endoscopic Sinus Surgery offers precise and complete removal of polyps. Image guided surgery increase the safety index during endoscpoic sinus surgery. In future, the key to successful management of nasal polyps will be an understanding of the underlying mucosa inflammation, mechanism of polyp formation and the genetic control of etiopathogenesis of nasal polyps..
Dr. V. P. Sood New Delhi.
Past President : Association of Otolaryngologists of India.
Past President : All India Rhinology Society.
Although patients with nasal polyps are common in E.N.T. practice but the aetiology of this condition still remains a mystery. The etiopathogenesis of nasal polyps has long been a subject of study, yet there is little agreement as to the mechanism of polyp formation. So far two main theories have emerged, allergic & infectious. Recently, sensitivity to aspirin and fungal infections have also been implicated as etiologic factors. Nasal polyps has been referred to as "benign allergic polyps" but research suggests that they are not more common in allergic patients. But now allergy has again been considered and there is a possibility that localized nasal allergy may have a role in the aetiology of polyps. The role of fungal infection in the aetiology of nasal polyps has been the source of great debate amongst rhinologists, since allergic fungal sinusitis has recently come to limelight.
In long standing infective polyposis most of the time there is bony necrosis of medial wall of maxillary sinus, lamina papyracia, ethmoid cells and anterior wall of the sphenoid sinuses. Chronic infective polyps degenerate to form into cheesy and muddy material, a condition referred to as necrotising ethmoiditis which should rather be called necrotising sinusitis since disease process is not only localized to ethmoid sinuses but can involve all the sinuses. The extent of endoscopic surgery should be planned and adapted to the requirement of individual cases. For circumscribed pathology minimum invasive endoscopic interventions are indicated. For diffuse polyposis of all sinuses a complete endoscopic ethmoidectomy together with the fenestration of the frontal, sphenoidal and maxillary sinuses is done. The disease is cleared from within the sinus cavities through the enlarged opening of the respective sinus. The end result should be as open ethmoidal cavity lined by moist mucosa and having free communication with the frontal, sphenoidal and maxillary sinuses. In multiple nasal polyps initial clearing is generally done with the help of microdebrider. Surgical results improve by carefull pre-operative planing, use of systemic antibiotics and steroids pre and post operatively. Use of thru-cut forceps and microdebrider also helps to preserve mucosa to achieve better results. Reconstructing adequate antrostomy is also conductive for better results. In diffuse polyposis a short course of systemic steroids pre operatively and post operatively is mandatory followed by topical steroid sprays.
Local application of amphotercin-B is now used especially when polyps are associated with fungal infections. Even in extensive polyposis, I prefer to do endoscopic sinus surgery under L.A. because the pupillary reflexes can be monitored and patient's subjective feedback of excessive pain sensation when the instruments are touching the orbital plate, cribriform plate or fovea ethmoidalis can be warning signals to the surgeon, which increase the safety index in endoscopic sinus surgery. I follow up my patients endoscopically for suction clearance of crusts and discharge. If I find any adhesion in middle meatus that is incised. If any small polyp is visible that is also removed without any pain or discomfort to the patient.
The follow up of patients in our country is poor. Patient must be told about importance of follow up. Modem technology, CT scanning and endoscopy enables us to make an early and appropriate diagnosis of nasal polyposis and Endoscopic Sinus Surgery offers precise and complete removal of polyps. Image guided surgery increase the safety index during endoscpoic sinus surgery. In future, the key to successful management of nasal polyps will be an understanding of the underlying mucosa inflammation, mechanism of polyp formation and the genetic control of etiopathogenesis of nasal polyps..
Sphenoid sinus: anatomy and surgery
The sphenoid sinus is the most posterior, median and inferior paranasal cavity embedded within the skull base.
• Its pneumatization is variable :
• Conchal — 5%; Pre-sellar — 25%; Post-sellar — 70%
• its walls are irregular: more pneumatized is the sphenoid sinus, more irregular are its walls.
• The intersinus septum is sagittal but rarely median.
• Its ostium is in the sphenoethmoidal recess.
• The anterior wall is at 7 cm from the anterior nasal spine and the posterior wall at 9 cm. One of the best landmarks of the anterior wall of the sphenoid sinus is the posterior wall of the maxillary sinus.
• The angulation between the rostrum and the floor of the nasal cavity is about 30'.
• The surrounding vital structures are numerous:
• Superiorly are : the pituitary fossa, the optic chiasma, the planum sphenoklale. the olfactory pathways and the frontal lobe
• Laterally are the internal carotid artery, the optic nerve, the caroticooptic recess, the cavernous sinus with the cranial nerves (III, IV, V, VI) and VI and V2
• The sinus was neglected for a long period of time because of its deep location within the skull, the subtle presentation of the pathology and the difficulty to reach it before the advent of the endonasal microsurgery.
• Now we must admit that the pathology is extremely various: it has been depicted by the imaging (CT and MRI)
• Infectious diseases : • Bacterial: acute: non complicated and complicated • Fungal — non invasive (fungus ball — AFS) — invasive forms • Inflammatory diseases: • Chronic sinusitis • Fungus-like sinusitis • Tumor • Sphenochoanal polyp • Inverted papilloma • Carcinoma — primary or extended from the rhinopharynx of the ethmoid sinus • Postoperative diseases : sinusitis and mucoceles • Traumatic diseases — CSF leakage • From a surgical point of view, it is the nasal gateway to the skull base (sella and parasellar regions).
SURGICAL ROUTES There are 5 different endonasal routes to the sphenoid sinus:
1. The transseptal approach
2. The paraseptal approach
3. The endonasal approach
4. The transethmoidal approach
5. The transpterygoid approach
The transseptal approach: This is the oldest one, commonly used by the neurosurgeons in case of pituitary tumor surgery. It needs a hemitransfixiant or sublabial incision. Then there is the elevation of mucoperichondrial flaps. A resection of the perpendicular plate of the ethmoid is then performed, with further visualisation of the sphenoid rostrum. The anterior walls of the sphenoid sinuses are then perforated with an aspirator or a straight forceps. All the anterior walls and the intersinus septum should be resected with a bone rongeur. Relations between the intersinus septum and the lateral wall must be checked on the CT present in the OR. This is an excellent median and bilateral approach for the sphenoid sinuses, particularly recommended in case of disturbed anatomy, thick bony walls, unique sphenoid sinus and median pathology.
The posterior transseptal approach or paraseptal approach The concept is to give a view on both sphenoid sinuses. The incision of the mucosa is made 1 cm posterior to the bony-cartilaginous junction of the nasal septum; Mucoperichondrial flaps are then elevated upto the rostrum. The posterior septum is resected. Then the sphenoid sinuses are opened bilaterally as previously described. The advantages are to limit the dissection of the columella and the cartilagineous part of the septum. Therefore there is no risk of saddle nose, displacement or septal hematoma. The resection of the posterior septum gives some crusts for a couple of weeks but there is no risk of development of atrophic rhinitis, osteitis or empty nose syndrome.
The endonasal approach: This is a pure endoscopic route. After putting some cottonoids soaked with adrenalin, the middle turbinate is visualized and displaced laterally. Then identification and resection of the superior turbinate must be done. The ostium of the sphenoid sinus is in the sphenoethmoidal recess, along the tail of the superior turbinate, which is a relevant landmark. The perforation of the anterior wall of the sinus must be done superiorly. Then the resection of the anterior wall is done with a bone rongeur. Attention must be paid not to elevate the mucosa. This leads to the development of fibrosis with subsequent closure of the opening. The resection should not be too inferior because the septal branch of the sphenopalatine artery runs along the anterior wall of the sphenoid sinus. If it bleeds, cauterisation with a bipolar cautery must be done. The author does not routinely cut the middle turbinate or its tail when he opens the sphenoid sinus. This approach is the safest one as it is median and inferior, far from the lateral wall.
The transethmoid approach: This is a variant of the later. The surgery begins with a complete opening of the ethmoid air cells up to the Onodi cell. Attention must be paid to the possible relation between the posterior ethmoid air cell and the optic nerve. Direct injury of the optic nerve has been described during dissection in the Onodi cell when the dissection is too close to the lamina papyracea. When the ethmoid sinus is large, the sphenoid sinus can be opened with a curette going inferiorly and medially. It is like a stair: we must go down to penetrate into the sphenoid sinus. When clear landmarks are missing, the endonasal route is safer with identification and resection of the tail of the superior turbinate.
• Its pneumatization is variable :
• Conchal — 5%; Pre-sellar — 25%; Post-sellar — 70%
• its walls are irregular: more pneumatized is the sphenoid sinus, more irregular are its walls.
• The intersinus septum is sagittal but rarely median.
• Its ostium is in the sphenoethmoidal recess.
• The anterior wall is at 7 cm from the anterior nasal spine and the posterior wall at 9 cm. One of the best landmarks of the anterior wall of the sphenoid sinus is the posterior wall of the maxillary sinus.
• The angulation between the rostrum and the floor of the nasal cavity is about 30'.
• The surrounding vital structures are numerous:
• Superiorly are : the pituitary fossa, the optic chiasma, the planum sphenoklale. the olfactory pathways and the frontal lobe
• Laterally are the internal carotid artery, the optic nerve, the caroticooptic recess, the cavernous sinus with the cranial nerves (III, IV, V, VI) and VI and V2
• The sinus was neglected for a long period of time because of its deep location within the skull, the subtle presentation of the pathology and the difficulty to reach it before the advent of the endonasal microsurgery.
• Now we must admit that the pathology is extremely various: it has been depicted by the imaging (CT and MRI)
• Infectious diseases : • Bacterial: acute: non complicated and complicated • Fungal — non invasive (fungus ball — AFS) — invasive forms • Inflammatory diseases: • Chronic sinusitis • Fungus-like sinusitis • Tumor • Sphenochoanal polyp • Inverted papilloma • Carcinoma — primary or extended from the rhinopharynx of the ethmoid sinus • Postoperative diseases : sinusitis and mucoceles • Traumatic diseases — CSF leakage • From a surgical point of view, it is the nasal gateway to the skull base (sella and parasellar regions).
SURGICAL ROUTES There are 5 different endonasal routes to the sphenoid sinus:
1. The transseptal approach
2. The paraseptal approach
3. The endonasal approach
4. The transethmoidal approach
5. The transpterygoid approach
The transseptal approach: This is the oldest one, commonly used by the neurosurgeons in case of pituitary tumor surgery. It needs a hemitransfixiant or sublabial incision. Then there is the elevation of mucoperichondrial flaps. A resection of the perpendicular plate of the ethmoid is then performed, with further visualisation of the sphenoid rostrum. The anterior walls of the sphenoid sinuses are then perforated with an aspirator or a straight forceps. All the anterior walls and the intersinus septum should be resected with a bone rongeur. Relations between the intersinus septum and the lateral wall must be checked on the CT present in the OR. This is an excellent median and bilateral approach for the sphenoid sinuses, particularly recommended in case of disturbed anatomy, thick bony walls, unique sphenoid sinus and median pathology.
The posterior transseptal approach or paraseptal approach The concept is to give a view on both sphenoid sinuses. The incision of the mucosa is made 1 cm posterior to the bony-cartilaginous junction of the nasal septum; Mucoperichondrial flaps are then elevated upto the rostrum. The posterior septum is resected. Then the sphenoid sinuses are opened bilaterally as previously described. The advantages are to limit the dissection of the columella and the cartilagineous part of the septum. Therefore there is no risk of saddle nose, displacement or septal hematoma. The resection of the posterior septum gives some crusts for a couple of weeks but there is no risk of development of atrophic rhinitis, osteitis or empty nose syndrome.
The endonasal approach: This is a pure endoscopic route. After putting some cottonoids soaked with adrenalin, the middle turbinate is visualized and displaced laterally. Then identification and resection of the superior turbinate must be done. The ostium of the sphenoid sinus is in the sphenoethmoidal recess, along the tail of the superior turbinate, which is a relevant landmark. The perforation of the anterior wall of the sinus must be done superiorly. Then the resection of the anterior wall is done with a bone rongeur. Attention must be paid not to elevate the mucosa. This leads to the development of fibrosis with subsequent closure of the opening. The resection should not be too inferior because the septal branch of the sphenopalatine artery runs along the anterior wall of the sphenoid sinus. If it bleeds, cauterisation with a bipolar cautery must be done. The author does not routinely cut the middle turbinate or its tail when he opens the sphenoid sinus. This approach is the safest one as it is median and inferior, far from the lateral wall.
The transethmoid approach: This is a variant of the later. The surgery begins with a complete opening of the ethmoid air cells up to the Onodi cell. Attention must be paid to the possible relation between the posterior ethmoid air cell and the optic nerve. Direct injury of the optic nerve has been described during dissection in the Onodi cell when the dissection is too close to the lamina papyracea. When the ethmoid sinus is large, the sphenoid sinus can be opened with a curette going inferiorly and medially. It is like a stair: we must go down to penetrate into the sphenoid sinus. When clear landmarks are missing, the endonasal route is safer with identification and resection of the tail of the superior turbinate.
The transplerygoid approach: This approach is far less used. It provides wide access on the lateral portion of the sphenoid sinus. It is indicated for the repair of a sphenoidal meningoencephalocele, lateral to the foramen rotundum. A middle antrostomy is performed. with visualization of the posterior wall of the maxillary sinus and the tail of the middle turbinate. The sphenopalatine artery coming from the sphenopalatine foramen must be identified and cut. The bone between the floor of the sphenoid sinus and the maxillary sinus must be drilled away. Inferiorly there is the pterygoid plate with the vidian canal. Sometimes the V2 can be identified. This approach is not easy to do as it exposes the content of the pterygopalatine fossa medially.
Sunday, August 17, 2014
Endoscopic classification of deviated nasal septum
Type 1 when you can see full middle turbinate, middle meatus.
Type 2 when only lateral part of middle turbinate can be seen only.
Type 3 when middle turbinate can't be seen at all.
Type 4 middle turbinate touching the lateral nasal wall.
Classification of middle turbinate pneumatization.
Three types of bulla concha pneumatization.
Lamellar
Bulbar
Total
Posterior ethmoidal artery bleed
Posterior ethmoid all artery bleed is more dangerous than anterior ethmoid all artery because of its proximity to optic nerve.
Swinging flashlight test is the test to diagnose this as this tests the compression on Optic nerve.
Saturday, August 16, 2014
Frontal sinus
Agger nasi is pneumatization of lacrimal bone.
For frontal sinus , u require 0.6 mm axial cuts with Sagittal and coronal reconstructions in 3D mode.
Frontal recess is like hourglass appearance.
As long as we see the floor of frontal sinus , it is sinus. When floor not seen, it is frontal recess.
Supra orbital cell is lateral and posterior to frontal sinus.
Good suction like liposuction unit suction increases the life of microdebrider three times.
PJ wormald suggested minimum size of 4 mm of frontal sinus opening but ideal is 8mm.
Balloon sinuplasty may not create this much size.
Thursday, August 14, 2014
Sunday, July 27, 2014
Superior laryngeal nerve palsy
This patient presented with four day history of hoarseness of voice. He was being treated for acute laryngitis by a physician. He was prescribed voice rest, antibiotics and antacids. He did not have any relief.
His laryngoscopy showed that his leafy vocal cord was bowing on adduction and did not have full tension. It was moving well but didn't close fully producing a significant vocal gap. A working diagnosis of left superior laryngeal nerve palsy was made and treatment started.
Friday, July 18, 2014
Contact Granuloma of the vocal cords
 |
| Blue arrow shows an active contact granuloma |
Monday, July 14, 2014
How common are symptomatic adenoids causing otitis media witheffusionin adult patients. ?
This 39 year gentleman presented with recurrent right side otitis media with effusion. Nasal endoscopy showed a mass in Nasopharynx blocking right side Eustachian tube. A MRI was done which suggested it to be Adenoids.a biopsy was also done which showed it to be reactive hyperplasia of lymphoid tissue.
Right side Grommet was put.
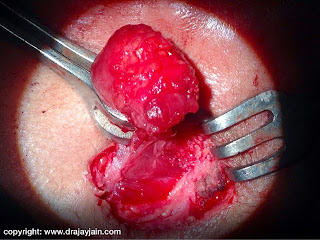
Cervical tuberculosis in a 8 year girl.
this 8 year girl presented with a mass just above hyoid bone. Pus was drained using a small incision and the mass become very firm with antibiotics treatment and did not disappear. the mass was excised under general anesthesia. It was very adherent to surrounding structures and bleeding a lot. Cheesy material was present in the core of the mass. It was thought to be a sebaceous cyst or thyroglossal cyst during surgery. Histopathological study report came as tuberculosis.
Subscribe to:
Comments (Atom)